
Using SEIR, a compartmental technique for epidemic analysis, researchers Nimra Hayat Nauraiz, and Ahmed Nauraiz Rana predict that by mid-May, 31.3 million (14% of the entire population) could contract the COVD-19 virus if effective mitigation and containment are not done. Urgent action is required in the coming weeks to bolster public health measures including distancing and beefing up the inadequate health infrastructure in the country.
A little over hundred years ago, the world was hit with a pandemic, well known as the Spanish influenza. While the source of the outbreak is unknown, the very first case was reported at a military base in Kansas on March 11, 1918. One would have expected India to encounter minimum exposure to this pandemic due to lack of geographic proximity, and mobility constraints, yet surprisingly 18 million people in India lost their lives, accounting for 6 percent of the country’s population at the time. According to health inspector J.S Turner, the disease “came like a thief in the night, its onset rapid and insidious,” infecting a third of the world’s population, and claiming up to 100 million lives.
The world back then was starkly different to the one we inhabit today in terms of inter-connectedness – much of the attributes of modern-day globalization, both physical and notional, barely existed. British India’s first civil aviation airport, Juhu Aerodrome, was not founded until 1928, indicative that the ability to readily travel to and from the subcontinent during the first quarter of the 20th century was not even remotely close to what it is now. Today, 11 cities in Pakistan accommodate international flight traffic, transporting on average 13 million passengers annually, rendering the country much more exposed to large-scale outbreaks of infectious diseases.
As the world grapples with Covid-19, experiencing an exponential surge in the number of people infected, it is important to highlight that this spread can well be attributed to increased global travel and integration, and urbanization. Pakistan is no exception, making the country as receptive and vulnerable to the virus, as any other. According to data from Pakistan’s Civil Aviation Authority, 20,026 international flight movements were recorded at Pakistan’s International airports between December 13, 2019 and March 13, 2020, a period during which Covid-19 was discovered, validated, and declared as a pandemic, encapsulating 171 countries in the word, and infecting over 200,000 people globally.
With Covid-19 lapping at Pakistan’s crowded cities, there is probable cause to expect that the world’s sixth most populous country may again bear a disproportionate share of global agony. Back in 1918, the sub-continent of India had a population of almost 300 million, with a population density of less than 500 people per square miles. Today Pakistan, alone, supports a population of over 210 million, with a density of 742 people per square miles. Evidence suggests that larger and denser populations only act to expedite the expansionary trajectory that viruses belonging to the Corona family assume.
Given the global spread, and models of predictive analysis, it can be claimed with certainty that the number of under-diagnosed cases in Pakistan is much greater than the one being reported – as is the case in almost every other country due to limited testing capability and the incubation period of the virus itself. The lack of urgency being exhibited by Pakistan’s administration and majority population in dealing with this pandemic, makes it all the more important to calculate, or at the very least estimate the number of people who have been infected and how many more are likely to be – highlighting the severity of the catastrophe that awaits.
This is what we did by leveraging the SEIR (Susceptible-Exposed-Infectious-Removed) model to estimate and project the spread of Covid-19 in Pakistan. SEIR is a compartmental technique used for epidemic analysis to ascertain how a disease spreads through a population. For our analysis, we used parameter estimates like incubation and infectious period from World Health Organization’s most recent study on Covid-19 (Hellewell et al. 2020) and used the reproduction number (R-naught) as that of the SARS-CoV virus, 4 (R-naught is the rate used to decipher an outbreak’s transmissibility; an R-naught of 4 implies that an infected person will further infect 4 individuals).
Covid-19 was carried by multiple individuals travelling to different parts of Pakistan from around the world. The exposure that each of the provinces had to Covid-19, in the initial phase of infection, varied from one another. Therefore, we tailored our model to determine the spread in each of Pakistan’s provinces based on their exposure (number of initial infections), total population and density, first date of contact, and the average population contact rate. The table below summarizes the estimated number of Covid-19 “actual” cases today, and how they are likely to increase in the absence of aggressive containment measures:
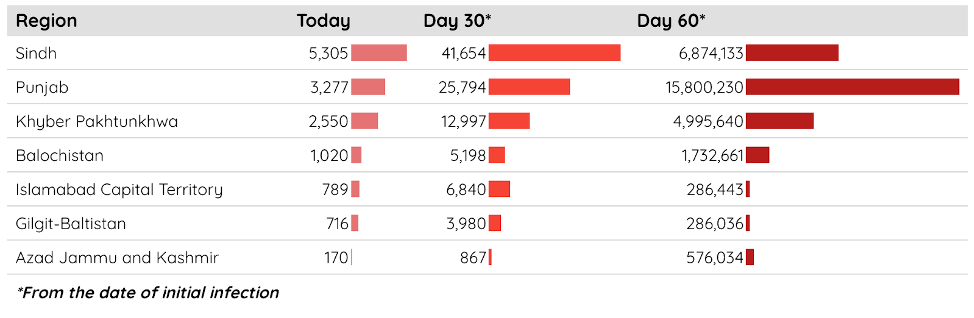
Punjab being Pakistan’s most populous and dense province, will encounter rapid acceleration and maximum spread of the virus, with the number of cases rising to a jolting 15 million by day 60. T
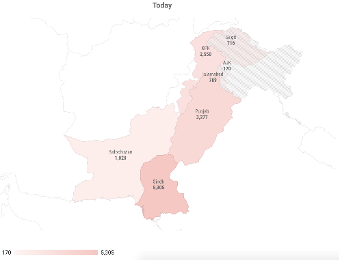
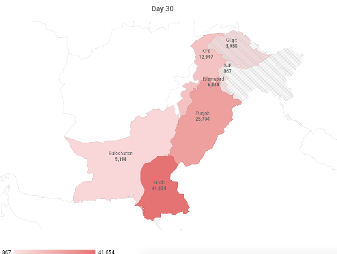
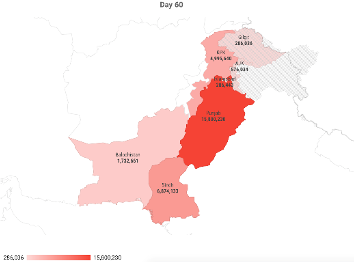
The following heat maps reflect the actual number of infectious cases across each province today (current day scenario), on day 30, and day 60, based on our estimation.
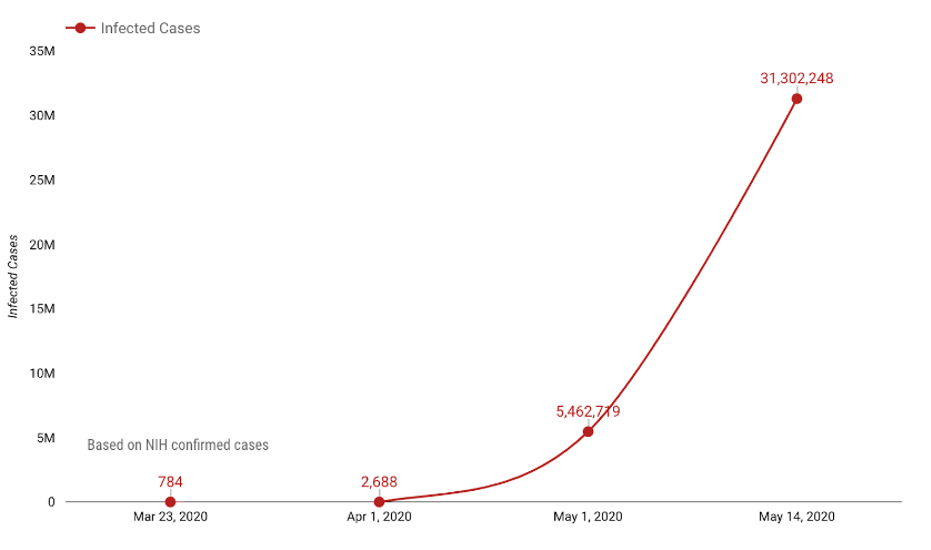
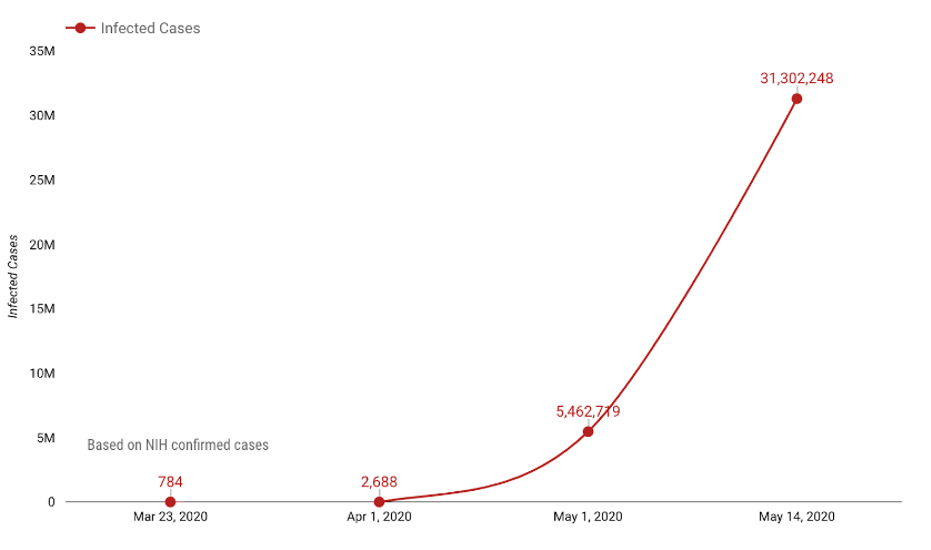
Assuming that the actual number of cases in Pakistan equals the number of officially “confirmed” cases by the NIH as of March 23, 2020 (which even by a stretch of imagination is far from being possible), we were able to predict that the country will see an exponential growth in the total number of infected individuals, in case a strategy to mitigate the spread was not employed, effectively and immediately . Following this trajectory, by mid-May, 31.3 million (14% of the entire population) will have contracted the virus.
The growth trajectory of Covid-19 infected cases in Pakistan is much aggressive than what was previously anticipated. The results are harrowing, as they should be, yet not surprising. The virus has indeed slipped past Pakistan’s barriers, dimming the prospects for stomping out the outbreak in its early stages; left unchecked it will continue to sweep the country. What makes Covid-19 way more dangerous than previous strains of viruses belonging to the Corona family is its insidiousness – the virus spreads quickly and silently, with people transmitting the disease without displaying any symptoms.
Additionally, the challenge to rightly identify and take timely measures is significantly impeded due to limited laboratory-testing capacity in Pakistan. Without adequate testing of the virus there can be no isolation of existing cases, and the chain of infection cannot be broken, as emphasized by WHO’s head, Tedros Adhanom Ghebreyesus, “Test, test, test. All countries should be able to test all suspected cases, they cannot fight this pandemic blindfolded.”
Given the state of Pakistan’s health infrastructure, based on decades of under-investment in public health – with the recent most budget being a meagre 0.53% of GDP – Pakistan is all the more exposed to the disastrous impact of Covid-19. According to the Global Health Security (GHS) index, which is a measure of country’s preparedness to deal with a pandemic, Pakistan scores 35.5, placing it even below Iran – a country expecting over a million deaths by the time the outbreak is over.
While the fatality rate of Covid-19 varies between 0.8% to 6% as of current global figures, it depends primarily on the quality of care a country can provide and the number of people who have access to it. This puts Pakistan in a glaringly dire position, given the unsurmountable gap between the health sector’s capacity to accommodate incoming patients and the number of people who are likely to be infected. Simply put, if those infected require intensive care, and it cannot be provided – majority will die.
The public is not well prepared either, nor is it aware of the imminent threat. There is widespread poverty which makes it practically impossible for many to leave jobs or work from home, but what exacerbates this astronomical situation is the population’s whimsical opinion regarding the perceived ‘non-severity,’ and the penchant for engaging in colossal ‘non-essential’ events. The urgency of the situation requires much disruptive measures, starting with stringent social distancing and isolation protocols – this will not help rid the country of Covid-19, but will dampen the wave of deaths. Lock down, as the one being imposed in Pakistan, will indeed suppress the growth rate of infection, but will not deter its resurgence (we aim to address this phenomenon and the impact of social distancing in our next piece).
There are many differences between 1918 and 2020: Pakistan is no longer a part of India; the sub-continent is no longer governed by the British; the Coronavirus is not the same as the Spanish Flu despite exhibiting similar symptoms; and more importantly, we know much more of modern medicine than we ever have. Yet, despite these caveats, much can be learned from the 1918 outbreak of influenza in India – a historical reservoir that illustrates, in painful detail, the outcome when an unprepared developing country is exposed to a virulent pandemic.
Nimra is a Data Scientist, who works with the New York Times; she tweets @nimramallick.
Nauraiz is a Development Economist based in Washington DC; he tweets @nauraizrana.
(The research carried out by the authors, and the opinion expressed is solely their own. It does not in any way reflect the viewpoint or findings of their respective organizations)
A little over hundred years ago, the world was hit with a pandemic, well known as the Spanish influenza. While the source of the outbreak is unknown, the very first case was reported at a military base in Kansas on March 11, 1918. One would have expected India to encounter minimum exposure to this pandemic due to lack of geographic proximity, and mobility constraints, yet surprisingly 18 million people in India lost their lives, accounting for 6 percent of the country’s population at the time. According to health inspector J.S Turner, the disease “came like a thief in the night, its onset rapid and insidious,” infecting a third of the world’s population, and claiming up to 100 million lives.
The world back then was starkly different to the one we inhabit today in terms of inter-connectedness – much of the attributes of modern-day globalization, both physical and notional, barely existed. British India’s first civil aviation airport, Juhu Aerodrome, was not founded until 1928, indicative that the ability to readily travel to and from the subcontinent during the first quarter of the 20th century was not even remotely close to what it is now. Today, 11 cities in Pakistan accommodate international flight traffic, transporting on average 13 million passengers annually, rendering the country much more exposed to large-scale outbreaks of infectious diseases.
As the world grapples with Covid-19, experiencing an exponential surge in the number of people infected, it is important to highlight that this spread can well be attributed to increased global travel and integration, and urbanization. Pakistan is no exception, making the country as receptive and vulnerable to the virus, as any other. According to data from Pakistan’s Civil Aviation Authority, 20,026 international flight movements were recorded at Pakistan’s International airports between December 13, 2019 and March 13, 2020, a period during which Covid-19 was discovered, validated, and declared as a pandemic, encapsulating 171 countries in the word, and infecting over 200,000 people globally.
With Covid-19 lapping at Pakistan’s crowded cities, there is probable cause to expect that the world’s sixth most populous country may again bear a disproportionate share of global agony. Back in 1918, the sub-continent of India had a population of almost 300 million, with a population density of less than 500 people per square miles. Today Pakistan, alone, supports a population of over 210 million, with a density of 742 people per square miles. Evidence suggests that larger and denser populations only act to expedite the expansionary trajectory that viruses belonging to the Corona family assume.
Given the global spread, and models of predictive analysis, it can be claimed with certainty that the number of under-diagnosed cases in Pakistan is much greater than the one being reported – as is the case in almost every other country due to limited testing capability and the incubation period of the virus itself. The lack of urgency being exhibited by Pakistan’s administration and majority population in dealing with this pandemic, makes it all the more important to calculate, or at the very least estimate the number of people who have been infected and how many more are likely to be – highlighting the severity of the catastrophe that awaits.
This is what we did by leveraging the SEIR (Susceptible-Exposed-Infectious-Removed) model to estimate and project the spread of Covid-19 in Pakistan. SEIR is a compartmental technique used for epidemic analysis to ascertain how a disease spreads through a population. For our analysis, we used parameter estimates like incubation and infectious period from World Health Organization’s most recent study on Covid-19 (Hellewell et al. 2020) and used the reproduction number (R-naught) as that of the SARS-CoV virus, 4 (R-naught is the rate used to decipher an outbreak’s transmissibility; an R-naught of 4 implies that an infected person will further infect 4 individuals).
Covid-19 was carried by multiple individuals travelling to different parts of Pakistan from around the world. The exposure that each of the provinces had to Covid-19, in the initial phase of infection, varied from one another. Therefore, we tailored our model to determine the spread in each of Pakistan’s provinces based on their exposure (number of initial infections), total population and density, first date of contact, and the average population contact rate. The table below summarizes the estimated number of Covid-19 “actual” cases today, and how they are likely to increase in the absence of aggressive containment measures:
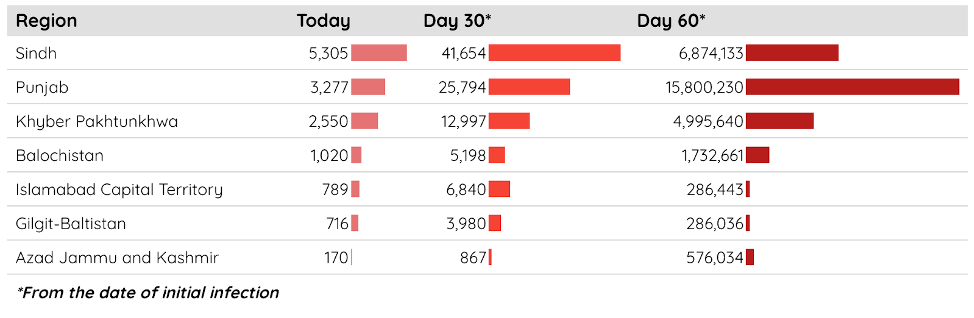
Punjab being Pakistan’s most populous and dense province, will encounter rapid acceleration and maximum spread of the virus, with the number of cases rising to a jolting 15 million by day 60. T
The following heat maps reflect the actual number of infectious cases across each province today (current day scenario), on day 30, and day 60, based on our estimation.
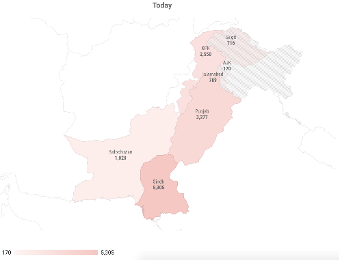
Today
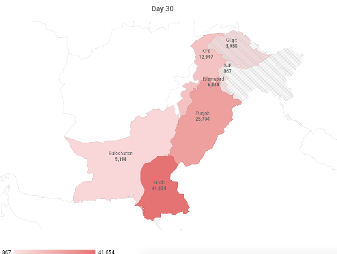
Day 30
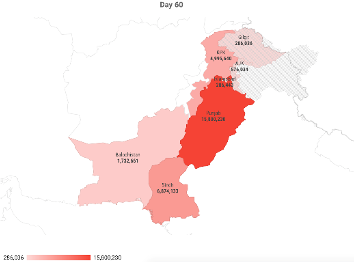
Day 60
Assuming that the actual number of cases in Pakistan equals the number of officially “confirmed” cases by the NIH as of March 23, 2020 (which even by a stretch of imagination is far from being possible), we were able to predict that the country will see an exponential growth in the total number of infected individuals, in case a strategy to mitigate the spread was not employed, effectively and immediately . Following this trajectory, by mid-May, 31.3 million (14% of the entire population) will have contracted the virus.
The growth trajectory of Covid-19 infected cases in Pakistan is much aggressive than what was previously anticipated. The results are harrowing, as they should be, yet not surprising. The virus has indeed slipped past Pakistan’s barriers, dimming the prospects for stomping out the outbreak in its early stages; left unchecked it will continue to sweep the country. What makes Covid-19 way more dangerous than previous strains of viruses belonging to the Corona family is its insidiousness – the virus spreads quickly and silently, with people transmitting the disease without displaying any symptoms.
Additionally, the challenge to rightly identify and take timely measures is significantly impeded due to limited laboratory-testing capacity in Pakistan. Without adequate testing of the virus there can be no isolation of existing cases, and the chain of infection cannot be broken, as emphasized by WHO’s head, Tedros Adhanom Ghebreyesus, “Test, test, test. All countries should be able to test all suspected cases, they cannot fight this pandemic blindfolded.”
Given the state of Pakistan’s health infrastructure, based on decades of under-investment in public health – with the recent most budget being a meagre 0.53% of GDP – Pakistan is all the more exposed to the disastrous impact of Covid-19. According to the Global Health Security (GHS) index, which is a measure of country’s preparedness to deal with a pandemic, Pakistan scores 35.5, placing it even below Iran – a country expecting over a million deaths by the time the outbreak is over.
While the fatality rate of Covid-19 varies between 0.8% to 6% as of current global figures, it depends primarily on the quality of care a country can provide and the number of people who have access to it. This puts Pakistan in a glaringly dire position, given the unsurmountable gap between the health sector’s capacity to accommodate incoming patients and the number of people who are likely to be infected. Simply put, if those infected require intensive care, and it cannot be provided – majority will die.
The public is not well prepared either, nor is it aware of the imminent threat. There is widespread poverty which makes it practically impossible for many to leave jobs or work from home, but what exacerbates this astronomical situation is the population’s whimsical opinion regarding the perceived ‘non-severity,’ and the penchant for engaging in colossal ‘non-essential’ events. The urgency of the situation requires much disruptive measures, starting with stringent social distancing and isolation protocols – this will not help rid the country of Covid-19, but will dampen the wave of deaths. Lock down, as the one being imposed in Pakistan, will indeed suppress the growth rate of infection, but will not deter its resurgence (we aim to address this phenomenon and the impact of social distancing in our next piece).
There are many differences between 1918 and 2020: Pakistan is no longer a part of India; the sub-continent is no longer governed by the British; the Coronavirus is not the same as the Spanish Flu despite exhibiting similar symptoms; and more importantly, we know much more of modern medicine than we ever have. Yet, despite these caveats, much can be learned from the 1918 outbreak of influenza in India – a historical reservoir that illustrates, in painful detail, the outcome when an unprepared developing country is exposed to a virulent pandemic.
Nimra is a Data Scientist, who works with the New York Times; she tweets @nimramallick.
Nauraiz is a Development Economist based in Washington DC; he tweets @nauraizrana.
(The research carried out by the authors, and the opinion expressed is solely their own. It does not in any way reflect the viewpoint or findings of their respective organizations)
